| Active substance | Minocycline (C23H27N3O7) |
| US Brand | Minocin, Minomycin, Akamin |
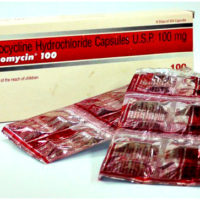
| IN Brand | Cynomicyn |
| Manufacturing by | Wyeth Limited |
| Strength | 50mg, 100mg |
| Form release | blister 12 capsules |
| Estimated shipping time | 7 – 18 days (Depending from the Country) |
| Availability, Prices & Order | through request form |
Minocycline is a tetracycline antibiotic that fights bacteria in the body.
Minocycline is used to treat many different bacterial infections, such as urinary tract infections, respiratory infections, skin infections, severe acne, gonorrhea, tick fever, chlamydia, and others.
Minocycline is a broad-spectrum tetracycline antibiotic, and has a broader spectrum than the other members of the group. It is a bacteriostatic antibiotic, classified as a long-acting type. As a result of its long half-life it generally has serum levels 2–4 times that of the simple water-soluble tetracyclines.
Minocycline is the most lipid-soluble of the tetracycline-class antibiotics, giving it the greatest penetration into the prostate and brain, but also the greatest amount of central nervous system (CNS)-related side effects, such as vertigo. A common side effect is diarrhea. Uncommon side effects (with prolonged therapy) include skin discolouration and autoimmune disorders that are not seen with other drugs in the class.
Minocycline is a relatively poor tetracycline-class antibiotic choice for urinary pathogens sensitive to this antibiotic class, as its solubility in water and levels in the urine are less than all other tetracyclines. Minocycline is metabolized by the liver and has poor urinary excretion.
Minocycline was patented in 1961 and came into commercial use in 1971. is not a naturally occurring antibiotic, but was synthesized semi-synthetically from natural tetracycline antibiotics by Lederle Laboratories in 1966, and marketed by them under the brand name Minocin.
Minocycline and doxycycline are frequently used for the treatment of acne vulgaris. Both of these closely related antibiotics have similar levels of efficacy, although doxycycline has a slightly lower risk of adverse side effects. Historically, minocycline has been a very effective treatment for acne vulgaris. However, acne that is caused by antibiotic resistant bacteria is a growing problem in many countries. In Europe and North America, a significant number of acne patients no longer respond well to treatment with tetracycline family antibiotics (e.g. tetracycline, doxycycline and minocycline) because their acne symptoms are caused by bacteria (primarily Propionibacterium acnes) that are resistant to these antibiotics.
Minocycline is also used for other skin infections such as MRSA as well as Lyme disease, as the one pill twice daily 100 mg dosage is far easier for patients than the four times a day required with tetracycline or oxytetracycline. Its activity against Lyme disease is enhanced by its superior ability to cross the blood-brain barrier.
Although minocycline’s broader spectrum of activity, compared with other members of the group, includes activity against Neisseria meningitidis,[12] its use as a prophylaxis is no longer recommended because of side effects (dizziness and vertigo).
It may be used to treat certain strains of MRSA infection and a disease caused by drug resistant Acinetobacter.
Both minocycline and doxycycline have shown effectiveness in asthma due to immune suppressing effects.[14] Minocycline as well as doxycycline have modest effectiveness in treating rheumatoid arthritis. It is recognized as a DMARD (Disease-Modifying Anti-Rheumatic Drug) by the American College of Rheumatology, which recommends its use as a treatment for rheumatoid arthritis.
A list of indications for which minocycline has been used include:
- Amoebic dysentery
- Anthrax
- Bubonic plague
- Cholera
- Ehrlichiosis
- Gonorrhea (when penicillin cannot be given)
- Gougerot-Carteaud syndrome (confluent and reticulated papillomatosis)
- Hidradenitis suppurativa
- HIV—for use as an adjuvant to HAART[16]
- Periodontal disease
- Perioral dermatitis[17]
- Respiratory infections such as pneumonia
- Rocky Mountain spotted fever
- Rosacea
- Syphilis (when penicillin cannot be given)
- Urinary tract infections, rectal infections, and infections of the cervix caused by certain microbes
Usual Adult Dose for Bacterial Infection
IV: 200 mg IV initially followed by 100 mg IV every 12 hours
Maximum dose: 400 mg/24 hours
Oral:
Most infections: 200 mg orally initially followed by 100 mg orally every 12 hours
-Alternative regimen (if more frequent dosing preferred): 100 to 200 mg orally initially followed by 50 mg orally 4 times a day
Uncomplicated urethral, endocervical, or rectal infections due to Chlamydia trachomatis or Ureaplasma urealyticum: 100 mg orally every 12 hours for at least 7 days
Comments:
-With trachoma, infectious agent is not always eliminated (as assessed by immunofluorescence).
-Coadministration with streptomycin recommended for bartonellosis.
-For syphilis, the duration of therapy is 10 to 15 days; close follow-up (including laboratory tests) recommended.
Uses:
-For the treatment of the following infections: Rocky Mountain spotted fever, typhus fever, typhus group, Q fever, rickettsialpox, tick fevers due to rickettsiae; respiratory tract infections due to Mycoplasma pneumoniae; lymphogranuloma venereum, trachoma, or inclusion conjunctivitis due to C trachomatis; psittacosis (ornithosis) due to Chlamydophila psittaci; nongonococcal urethritis, endocervical, or rectal infections due to U urealyticum or C trachomatis; relapsing fever due to Borrelia recurrentis; plague due to Yersinia pestis; tularemia due to Francisella tularensis; cholera due to Vibrio cholerae; Campylobacter fetus infections; brucellosis due to Brucella species; bartonellosis due to Bartonella bacilliformis; granuloma inguinale due to Klebsiella granulomatis
-For the treatment of infections due to the following bacteria when bacteriologic testing shows suitable susceptibility to this drug: Escherichia coli; Enterobacter aerogenes; Shigella species; Acinetobacter species; respiratory tract infections due to Haemophilus influenzae; respiratory tract and urinary tract infections due to Klebsiella species; upper respiratory tract infections due to Streptococcus pneumoniae
-When penicillin is contraindicated, as an alternative agent for the treatment of the following infections: Syphilis due to Treponema pallidum subspecies pallidum; yaws due to T pallidum subspecies pertenue; listeriosis due to Listeria monocytogenes; anthrax due to Bacillus anthracis; Vincent’s infection due to Fusobacterium fusiforme; actinomycosis due to Actinomyces israelii; clostridial infections
-As adjunctive therapy for: Acute intestinal amebiasis; severe acne
Usual Adult Dose for Acne
Extended-release formulations:
45 to 49 kg: 45 mg orally once a day
50 to 59 kg: 55 mg orally once a day
60 to 71 kg: 65 mg orally once a day
72 to 84 kg: 80 mg orally once a day
85 to 96 kg: 90 mg orally once a day
97 to 110 kg: 105 mg orally once a day
111 to 125 kg: 115 mg orally once a day
126 to 136 kg: 135 mg orally once a day
Duration of therapy: 12 weeks
Comments:
-Recommended dose is about 1 mg/kg once a day.
-This drug did not show any effect on non-inflammatory acne lesions.
-Safety not established beyond 12 weeks.
Use: To treat only inflammatory lesions of non-nodular moderate to severe acne vulgaris
American Academy of Dermatology (AAD) Recommendations:
Immediate-release formulations: 50 mg orally once to 3 times a day
Comments:
-Recommended as adjunctive treatment of moderate to severe inflammatory acne
-This drug should not be used as monotherapy.
-Use should be limited to the shortest duration possible; reevaluation recommended at 3 to 4 months to minimize resistant bacteria developing.
-Current guidelines should be consulted for additional information.
Usual Adult Dose for Meningitis – Meningococcal
200 mg IV initially followed by 100 mg IV every 12 hours
Maximum dose: 400 mg/24 hours
Use: When penicillin is contraindicated, as an alternative agent for the treatment of meningitis due to Neisseria meningitidis
Usual Adult Dose for Meningococcal Meningitis Prophylaxis
100 mg orally every 12 hours for 5 days
Comments:
-Diagnostic laboratory studies (including serotyping and susceptibility testing) are recommended to establish the carrier state and the appropriate therapy.
-Prophylactic use of this drug is only recommended when risk of meningococcal meningitis is high.
Use: In the treatment of asymptomatic carriers of N meningitidis to eliminate meningococci from the nasopharynx
Usual Adult Dose for Skin or Soft Tissue Infection
IV: 200 mg IV initially followed by 100 mg IV every 12 hours
Maximum dose: 400 mg/24 hours
Oral:
Infection due to Staphylococcus aureus: 200 mg orally initially followed by 100 mg orally every 12 hours
-Alternative regimen (if more frequent dosing preferred): 100 to 200 mg orally initially followed by 50 mg orally 4 times a day
Infection due to Mycobacterium marinum: 100 mg orally every 12 hours for 6 to 8 weeks
Comments:
-Not the drug of choice for any type of staphylococcal infection
-The optimal dose has not been established to treat M marinum infections; the recommended dose has been successful in limited cases.
Uses: For the treatment of skin and skin structure infections due to S aureus when bacteriologic testing shows suitable susceptibility to this drug; for the treatment of infections due to M marinum
Infectious Diseases Society of America (IDSA) Recommendations: 100 mg orally twice a day
Comments:
-Recommended for skin and soft tissue infections due to methicillin-susceptible and methicillin-resistant S aureus
-After an initial dose of 200 mg, recommended for purulent cellulitis (cellulitis associated with purulent drainage/exudate without a drainable abscess) due to methicillin-resistant S aureus
-Current guidelines should be consulted for additional information.
Minocycline may cause upset stomach, diarrhea, dizziness, unsteadiness, drowsiness, mouth sores, headache and vomiting. Minocycline increases sensitivity to sunlight. Minocycline may affect quality of sleep and rarely cause sleep disorders. It has also been linked to cases of lupus. Prolonged use of minocycline over an extended period of time can lead to blue-gray skin, fingernails and staining of scar tissue. This staining is not permanent but can take a very long time for the skin color to return to normal; on the other hand a muddy brown skin color in sun exposed areas is usually a permanent skin discolouration. Permanent blue discoloration of gums or teeth discoloration may also occur. Rare but serious side effects include fever, yellowing of the eyes or skin, stomach pain, sore throat, vision changes, and mental changes, including depersonalization.